Diabetes, or diabetes mellitus, is a chronic condition that affects millions of people worldwide. It occurs when the body is unable to effectively regulate blood sugar (glucose) levels, either due to insufficient insulin production or the body’s inability to use insulin properly. Insulin is a crucial hormone that helps the body convert sugar from the food we eat into energy. Without proper regulation, high blood sugar can lead to a range of health complications, affecting organs like the heart, kidneys, and eyes.
This guide aims to provide an in-depth understanding of diabetes, its types, causes, symptoms, treatment options, and ways to prevent it. Whether you’re newly diagnosed, managing diabetes, or want to learn how to reduce your risk, this comprehensive overview will equip you with the knowledge to take control of your health.
What is Diabetes?
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by consistently high blood sugar levels. This condition occurs when the body either doesn’t produce enough insulin or cannot use insulin effectively. Insulin is a hormone produced by the pancreas that allows glucose (sugar) from the food we eat to enter cells and be used for energy. Without adequate insulin function, glucose builds up in the bloodstream, leading to a range of health complications.

There are three primary types of diabetes:
- Type 1 Diabetes: Often diagnosed in childhood or adolescence, type 1 diabetes is an autoimmune disorder where the immune system attacks the insulin-producing cells in the pancreas. As a result, the body produces little or no insulin, and individuals with type 1 diabetes require insulin injections or pumps to manage their blood sugar levels.
- Type 2 Diabetes: The most common form of diabetes, type 2 occurs when the body becomes resistant to insulin or doesn’t produce enough of it. This type is often linked to lifestyle factors such as obesity, poor diet, and lack of exercise. It typically develops in adults but can occur at any age.
- Gestational Diabetes: This type occurs during pregnancy when hormonal changes make the body resistant to insulin. While gestational diabetes often resolves after childbirth, it increases the mother’s risk of developing type 2 diabetes later in life.
Understanding these key types of diabetes is essential for recognizing the unique causes and management strategies for each.
Types of Diabetes
Diabetes comes in several forms, with type 1 diabetes, type 2 diabetes, and gestational diabetes being the most common. Each type has unique causes, risk factors, and treatment strategies. Understanding the differences is crucial for effective management and prevention.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Without insulin, glucose cannot enter the cells, leading to elevated blood sugar levels. This form of diabetes often develops in childhood or adolescence, though it can appear at any age.
Symptoms of type 1 diabetes include excessive thirst, frequent urination, unexplained weight loss, extreme hunger, and fatigue. Since the body can no longer produce insulin, people with type 1 diabetes must rely on insulin therapy to regulate their blood sugar levels.
Type 2 Diabetes
Type 2 diabetes is a progressive condition where the body becomes resistant to insulin, meaning the cells do not respond effectively to the hormone. Over time, the pancreas may not produce enough insulin to keep blood sugar levels within a normal range. Unlike type 1, which is autoimmune, type 2 diabetes is largely associated with lifestyle factors, though genetics also play a significant role.
Risk factors for type 2 diabetes include obesity, a sedentary lifestyle, poor diet, and family history of diabetes. It typically develops in adults but is becoming more common in younger individuals due to rising obesity rates. Unlike type 1 diabetes, type 2 diabetes can often be managed with lifestyle changes such as diet, exercise, and sometimes medication or insulin therapy.
Gestational Diabetes
Gestational diabetes occurs during pregnancy when hormonal changes make the body more resistant to insulin. Although it often resolves after childbirth, women who develop gestational diabetes are at a higher risk of developing type 2 diabetes later in life.
Gestational diabetes is typically diagnosed through routine screening in the second trimester and can be managed with diet, exercise, and sometimes insulin or medication to ensure both the mother’s and baby’s health.
Difference Between Type 1 and Type 2 Diabetes
- Cause: Type 1 diabetes is an autoimmune disorder, while type 2 diabetes is primarily caused by insulin resistance and lifestyle factors.
- Onset: Type 1 diabetes often begins in childhood or adolescence, whereas type 2 diabetes generally develops in adulthood, though it is becoming more common in younger people.
- Management: Type 1 diabetes requires insulin for life, while type 2 diabetes can often be managed with lifestyle changes, oral medications, and, in some cases, insulin.
Causes and Risk Factors of Diabetes
Diabetes is influenced by a combination of genetic, environmental, and lifestyle factors. Understanding the specific causes and risk factors of each type of diabetes is essential for both prevention and management.
Type 1 Diabetes Causes
Type 1 diabetes is an autoimmune disease, meaning the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. The exact cause of this autoimmune response remains unclear, but it is believed that genetic predisposition plays a significant role. Environmental factors, such as viral infections, may also trigger the autoimmune reaction in individuals who are genetically susceptible.
While type 1 diabetes is often associated with genetics, not everyone with a family history will develop the condition. However, having a first-degree relative (such as a parent or sibling) with type 1 diabetes increases the likelihood of developing the disease.
Type 2 Diabetes Causes
Type 2 diabetes is primarily caused by insulin resistance, a condition in which the body’s cells do not respond properly to insulin. As a result, the pancreas produces more insulin to compensate, but over time, it may not be able to keep up, leading to elevated blood sugar levels.
Several lifestyle factors contribute to the development of type 2 diabetes, including:
- Poor diet: Consuming high amounts of processed foods, refined sugars, and unhealthy fats can lead to weight gain and insulin resistance.
- Lack of physical activity: A sedentary lifestyle contributes to weight gain and can exacerbate insulin resistance.
- Obesity: Being overweight, particularly with excess abdominal fat, is a major risk factor for insulin resistance and type 2 diabetes.
In addition to lifestyle factors, genetics can play a role. Having a family history of type 2 diabetes increases the risk of developing the condition, though it can often be prevented or delayed with lifestyle modifications.
Gestational Diabetes Causes
Gestational diabetes occurs during pregnancy due to hormonal changes that make the body more resistant to insulin. The placenta produces hormones that interfere with the effectiveness of insulin, leading to elevated blood sugar levels. While gestational diabetes typically resolves after delivery, it can increase the mother’s risk of developing type 2 diabetes later in life.
Risk factors for gestational diabetes include:
- Being overweight or obese before pregnancy
- Family history of diabetes
- Previous gestational diabetes in an earlier pregnancy
- Being over the age of 25
Additional Risk Factors for All Types of Diabetes
- Family history: A genetic predisposition to diabetes can increase the likelihood of developing the condition.
- Age: The risk of type 2 diabetes increases with age, particularly after 45 years.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, Native Americans, and Asians, are at higher risk for type 2 diabetes.
- Prediabetes: What is prediabetes? It refers to a state where blood sugar levels are higher than normal but not high enough to be classified as diabetes. Prediabetes increases the risk of developing type 2 diabetes if lifestyle changes are not made.
Understanding these causes and risk factors can help individuals take proactive steps to prevent or manage diabetes effectively.
Common Symptoms of Diabetes
Diabetes can present with a variety of symptoms that are often related to elevated blood sugar levels. While some symptoms are common to both type 1 and type 2 diabetes, others may vary depending on the type of diabetes and the progression of the disease. Early recognition of these symptoms is crucial for timely diagnosis and management.

Common Symptoms of Diabetes
- Frequent urination (polyuria): Excess glucose in the blood forces the kidneys to work harder to filter and absorb it, resulting in increased urination as the body tries to eliminate the excess sugar.
- Excessive thirst (polydipsia): As a result of frequent urination, the body loses more fluids, leading to dehydration and increased thirst.
- Unexplained weight loss: Particularly common in type 1 diabetes, the body starts to break down fat and muscle for energy when it cannot use glucose due to the lack of insulin.
- Fatigue: When the body is unable to use glucose for energy efficiently, it can lead to constant tiredness and lack of energy.
- Blurred vision: High blood sugar can affect the shape and function of the eye’s lens, leading to blurry vision.
- Slow-healing sores: High glucose levels impair the body’s ability to heal wounds and fight infections, causing sores to heal more slowly.
- Numbness or tingling in hands or feet: Prolonged high blood sugar can lead to nerve damage (diabetic neuropathy), which often presents as numbness, tingling, or pain in the extremities.
Symptom Patterns in Type 1 vs. Type 2 Diabetes
- Type 1 Diabetes Symptoms:
Symptoms of type 1 diabetes tend to develop suddenly and are more severe due to the body’s inability to produce insulin. Unexplained weight loss and ketoacidosis (a serious condition that occurs when the body produces high levels of ketones due to fat breakdown) are more common in type 1 diabetes. People with type 1 diabetes are typically diagnosed in childhood or adolescence, although it can occur at any age. - Type 2 Diabetes Symptoms:
In contrast, type 2 diabetes symptoms develop gradually over time and may initially go unnoticed. Many individuals with type 2 diabetes may not experience obvious symptoms until the condition is well advanced. Fatigue, blurred vision, and numbness in the extremities are more common in type 2 diabetes due to prolonged high blood sugar and insulin resistance. In some cases, individuals may only discover they have type 2 diabetes after routine blood tests.
Recognizing the symptoms of diabetes, whether sudden or gradual, is critical for early diagnosis and intervention. If you or someone you know experiences any of these symptoms, it’s important to consult a healthcare professional for further evaluation.
How is Diabetes Diagnosed?
Diagnosing diabetes early is crucial for managing the condition and preventing complications. Various blood tests are used to diagnose diabetes and determine whether a person has prediabetes, type 1 diabetes, or type 2 diabetes. Each test measures how well the body regulates blood sugar levels and can provide insight into long-term glucose control.
Common Diagnostic Tests for Diabetes
- Fasting Blood Sugar Test
A fasting blood sugar test measures your blood glucose level after fasting (no food or drink except water) for at least 8 hours. It’s one of the simplest and most commonly used tests for diagnosing diabetes.- Normal: Less than 100 mg/dL
- Prediabetes: 100-125 mg/dL
- Diabetes: 126 mg/dL or higher on two separate tests
- HbA1c Test (Glycated Hemoglobin Test)
The HbA1c test, also known as the A1c test, provides an average of your blood sugar levels over the past 2-3 months. It measures the percentage of hemoglobin that is coated with sugar (glycated), reflecting your long-term glucose levels.- Normal: Less than 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher on two separate tests
- Oral Glucose Tolerance Test (OGTT)
The OGTT involves drinking a sugary solution, followed by measuring blood sugar levels at intervals to see how efficiently your body processes glucose. This test is particularly important for diagnosing gestational diabetes during pregnancy.- Normal: Less than 140 mg/dL after 2 hours
- Prediabetes: 140-199 mg/dL after 2 hours
- Diabetes: 200 mg/dL or higher after 2 hours
- Random Blood Sugar Test
A random blood sugar test can be done at any time of the day, regardless of when you last ate. A result of 200 mg/dL or higher, combined with symptoms of diabetes such as excessive thirst, frequent urination, or unexplained weight loss, can indicate diabetes.
Prediabetes Diagnosis
Prediabetes is a condition where blood sugar levels are higher than normal but not yet high enough to be classified as type 2 diabetes. Diagnosing prediabetes is crucial as it provides an opportunity to make lifestyle changes that can prevent or delay the onset of diabetes. The following results from diagnostic tests indicate prediabetes:
- Fasting blood sugar: 100-125 mg/dL
- HbA1c: 5.7% to 6.4%
- OGTT: 140-199 mg/dL after 2 hours
If you are diagnosed with prediabetes, your healthcare provider may recommend lifestyle changes, such as improving your diet, increasing physical activity, and possibly using medications to reduce your risk of progressing to type 2 diabetes.
Additional Tests for Type 1 Diabetes
In cases of suspected type 1 diabetes, additional tests may be done to check for the presence of autoantibodies, which are markers of the immune system attacking insulin-producing cells in the pancreas. C-peptide levels may also be measured to assess insulin production in the body.
Diagnosing diabetes early through these tests can lead to better management and prevent complications. If you experience symptoms or have risk factors for diabetes, speak to your doctor about testing options.
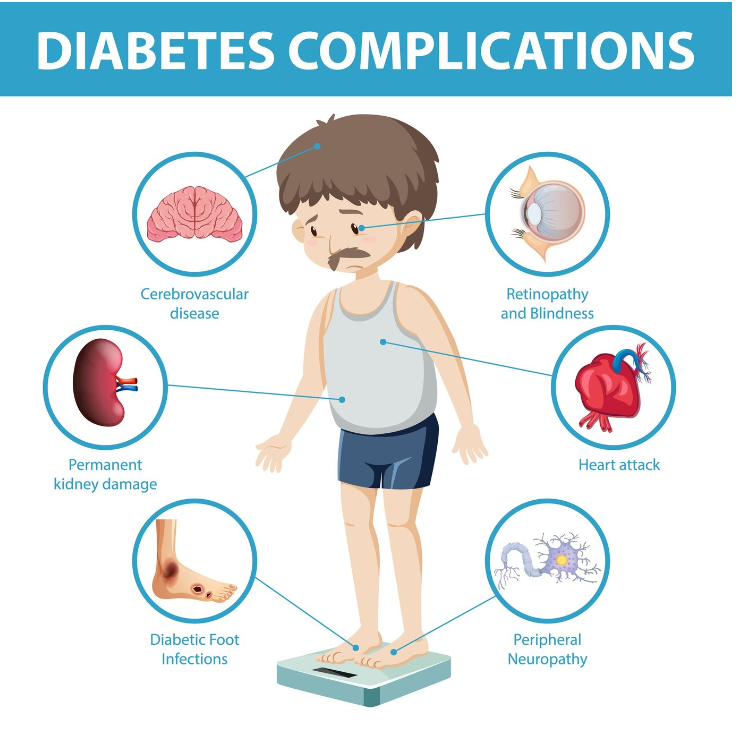
Complications of Diabetes
Unmanaged or poorly controlled diabetes can lead to a wide range of serious health complications that affect various organs and systems in the body. These complications often develop gradually over time but can become life-threatening if left untreated. Proper blood sugar management, early detection, and consistent monitoring are key to reducing the risk of these complications.
Common Complications of Diabetes
- Heart Disease and Stroke
Cardiovascular disease is one of the most common and severe complications of diabetes. High blood sugar levels can damage blood vessels and lead to an increased risk of heart attacks, strokes, and other cardiovascular problems. Individuals with diabetes are more likely to develop high blood pressure, high cholesterol, and atherosclerosis, which can further increase the risk of heart-related issues. - Diabetic Neuropathy
Diabetic neuropathy is nerve damage caused by prolonged high blood sugar levels. It most commonly affects the nerves in the hands and feet, leading to symptoms such as tingling, numbness, pain, and weakness. Severe cases of neuropathy can result in loss of sensation, increasing the risk of foot injuries, infections, and in extreme cases, amputations. - Diabetic Retinopathy
Diabetic retinopathy is a complication that affects the eyes and can lead to blindness if untreated. High blood sugar can damage the blood vessels in the retina, causing them to leak or become blocked. Over time, this damage can lead to vision problems, including blurry vision, floaters, or even complete vision loss. - Kidney Damage (Diabetic Nephropathy)
Diabetic nephropathy occurs when high blood sugar damages the kidneys’ delicate filtering system. This damage can lead to chronic kidney disease and eventually kidney failure. In advanced cases, patients may require dialysis or a kidney transplant. Keeping blood sugar levels in check and managing blood pressure are crucial in preventing kidney damage. - Foot Problems and Amputations
People with diabetes are prone to developing foot problems due to poor circulation and nerve damage (neuropathy). Even minor cuts, blisters, or sores can become infected and heal poorly. In severe cases, untreated infections can lead to gangrene, requiring amputation. Regular foot care and monitoring are essential to prevent such outcomes. - Increased Risk of Infections
Diabetes weakens the immune system, making it harder for the body to fight off infections. High blood sugar levels create an environment where bacteria and fungi thrive, increasing the risk of skin, urinary tract, and other types of infections. Proper blood sugar control helps reduce the frequency and severity of infections.
What Happens If Diabetes Is Untreated?
Untreated diabetes can result in severe long-term effects that impair quality of life and can be life-threatening. High blood sugar levels, over time, damage organs and tissues throughout the body, leading to the complications mentioned above. Uncontrolled diabetes can also cause:
- Ketoacidosis: A dangerous buildup of acids in the blood (in type 1 diabetes).
- Hyperosmolar hyperglycemic state: Extremely high blood sugar leading to dehydration, confusion, and potential coma (in type 2 diabetes).
Long-term Effects of Diabetes
In addition to specific complications, poorly managed diabetes can have other long-term effects, including:
- Cognitive decline: Research has shown that individuals with diabetes are at higher risk of developing dementia and Alzheimer’s disease.
- Hearing impairment: Diabetes can lead to hearing loss due to nerve damage in the auditory system.
- Skin conditions: Persistent high blood sugar can cause various skin issues, including bacterial and fungal infections, and conditions like diabetic dermopathy.
The Importance of Early Detection and Proper Management
Early detection of diabetes through routine screening and timely management can drastically reduce the risk of complications. By controlling blood sugar levels, maintaining a healthy lifestyle, and regularly visiting healthcare professionals, individuals with diabetes can prevent or delay many of these serious health outcomes.
Proper diabetes management involves:
- Consistent blood sugar monitoring
- Healthy eating and physical activity
- Medications or insulin therapy as prescribed
- Regular check-ups to monitor potential complications
Managing diabetes effectively helps maintain long-term health and significantly reduces the risk of life-altering complications.
Diabetes Treatment Options
Diabetes management is essential for maintaining blood sugar levels within a healthy range and preventing complications. While there is no complete cure for diabetes, effective treatment options exist that allow individuals to manage their condition and lead healthy lives. The treatment strategies differ depending on the type of diabetes, but all focus on balancing blood sugar levels through medications, lifestyle changes, and regular monitoring.
Type 1 Diabetes Treatment
For individuals with type 1 diabetes, the primary treatment involves insulin therapy, as their bodies do not produce insulin. Insulin is crucial for allowing glucose to enter the cells for energy, and without it, blood sugar levels rise dangerously. Type 1 diabetes patients must take insulin regularly to manage their condition.
- Types of Insulin:
Insulin comes in various forms, differing in how quickly they act and how long they last:- Short-acting insulin: Starts working quickly and is typically taken before meals.
- Long-acting insulin: Provides a steady release over 24 hours to maintain baseline insulin levels.
- Insulin Pumps:
Some individuals use insulin pumps, small devices that deliver a steady amount of insulin throughout the day, reducing the need for multiple daily injections. Pumps can also deliver additional insulin doses when eating, offering more control and flexibility in managing blood sugar levels.
Type 2 Diabetes Treatment
The treatment for type 2 diabetes usually begins with lifestyle changes and may include medications to help control blood sugar levels.
- Oral Medications:
One of the most common medications for type 2 diabetes is metformin, which helps reduce glucose production in the liver and improves the body’s sensitivity to insulin. Other medications are used if metformin is not enough to control blood sugar levels. These include:- Sulfonylureas: Help the pancreas produce more insulin.
- Thiazolidinediones: Improve insulin sensitivity in cells.
- Newer Treatments:
Recent advancements in diabetes treatment have introduced newer medications that are particularly effective in managing type 2 diabetes:- GLP-1 receptor agonists: These drugs, such as liraglutide and semaglutide, help stimulate insulin production and reduce appetite. They have been shown to support weight loss as well, which is beneficial for type 2 diabetes management.
- SGLT2 inhibitors: Drugs like dapagliflozin and empagliflozin work by helping the kidneys remove excess sugar from the body through urine. They also have cardiovascular and kidney-protective benefits, making them a valuable option for many patients.
- Lifestyle Changes:
Lifestyle modifications, including a healthy diet, regular exercise, and weight management, are fundamental in managing type 2 diabetes. These changes improve insulin sensitivity and help maintain blood sugar levels within the target range.
Gestational Diabetes Treatment
Gestational diabetes, which develops during pregnancy, requires careful monitoring to protect both the mother and baby. While this form of diabetes typically resolves after delivery, managing blood sugar levels during pregnancy is essential.
- Dietary Changes:
Women with gestational diabetes are usually advised to adopt a diet focused on whole grains, fruits, vegetables, and lean proteins while limiting sugar and processed foods. This helps maintain healthy blood sugar levels throughout the day. - Regular Monitoring:
Blood sugar levels need to be monitored frequently to ensure they remain within the recommended range. This is typically done using a glucose meter, allowing the mother to track her levels and make necessary adjustments. - Insulin Therapy:
In some cases, insulin may be required to maintain blood sugar control if lifestyle changes are not sufficient. Insulin is safe to use during pregnancy and helps prevent complications.
Can Diabetes Be Cured?
Although diabetes cannot be cured, particularly type 1 diabetes, there is hope for individuals with type 2 diabetes in terms of remission. Remission means that blood sugar levels return to a normal range without the need for medications, though this does not mean the person is completely cured. Remission can be achieved through significant weight loss, lifestyle changes, and sometimes bariatric surgery.
In type 2 diabetes, remission is most likely if the condition is diagnosed early and aggressive lifestyle interventions are implemented. However, continued monitoring is necessary to ensure blood sugar levels remain in the healthy range, as diabetes can return if these changes are not maintained.
In summary, while diabetes cannot be fully cured, it can be effectively managed with the right combination of treatment options, helping individuals maintain a healthy and active life.
Managing Diabetes: Lifestyle and Diet
Effectively managing diabetes involves more than just medications; it requires long-term lifestyle changes that support healthy blood sugar levels. A balanced diet, regular physical activity, and weight management all play a crucial role in keeping diabetes in check. Whether you have type 1 or type 2 diabetes, implementing these strategies can help you control the condition naturally.
Dietary Guidelines for Diabetes
The foundation of diabetes management is a well-balanced diet that promotes stable blood sugar levels. Making mindful food choices can greatly improve your ability to manage the condition naturally.
- High-Fiber Foods: Incorporating fiber-rich foods such as fruits, vegetables, legumes, and whole grains helps slow the absorption of sugar and prevents blood sugar spikes. Fiber also promotes heart health, which is especially important for people with diabetes.
- Whole Grains: Opt for whole grains like brown rice, quinoa, oats, and barley instead of refined carbohydrates. These foods have a lower glycemic index, meaning they have a smaller impact on blood sugar levels.
- Lean Proteins: Include lean proteins such as chicken, turkey, fish, tofu, and beans in your diet. Protein helps stabilize blood sugar levels and keeps you full for longer.
- Healthy Fats: Choose healthy fats like those found in avocados, nuts, seeds, and olive oil. These fats are beneficial for heart health and help improve insulin sensitivity.
Foods to Avoid:
While certain foods can be helpful for managing diabetes, others should be limited or avoided:
- Refined Sugars: Minimize the consumption of sugary drinks, sweets, and desserts that can cause rapid blood sugar spikes.
- Processed Carbohydrates: Limit intake of white bread, pasta, and pastries made from refined flour, as they can quickly elevate blood sugar levels.
By following a balanced diet rich in whole, unprocessed foods, you can improve your blood sugar control and overall health.
Physical Activity
Exercise is one of the most effective natural ways to manage diabetes. Physical activity helps the body use insulin more efficiently, lowers blood sugar levels, and contributes to overall health.
- Aerobic Exercise: Activities like walking, swimming, and cycling can help lower blood sugar and improve cardiovascular health. Aim for at least 150 minutes of moderate aerobic exercise per week, spread over several days.
- Strength Training: Lifting weights or doing body-weight exercises like push-ups or squats helps build muscle, which in turn improves insulin sensitivity and helps regulate blood sugar levels.
- Flexibility and Balance: Incorporate activities like yoga and stretching to improve flexibility and balance, which is especially important for preventing falls and maintaining mobility as you age.
Regular exercise can also boost your mood, reduce stress, and improve sleep quality—all of which are beneficial for managing diabetes.
Weight Management
Maintaining a healthy weight is particularly important for managing type 2 diabetes. Excess body fat, especially around the abdomen, can make your body more resistant to insulin, making it harder to control blood sugar levels. By losing weight, even a small percentage, you can improve insulin sensitivity and reduce the need for medications.
- Weight Loss: For individuals with type 2 diabetes, losing weight can help manage the condition more effectively, and in some cases, lead to remission. Weight loss can be achieved through a combination of a healthy diet and regular exercise.
- Can Diabetes Cause Weight Loss?
In some cases, unexplained weight loss can be a symptom of diabetes, particularly if blood sugar levels are not well-controlled. This happens when the body cannot use glucose for energy and begins breaking down muscle and fat stores. If you experience unexpected weight loss, it’s important to consult a healthcare provider for evaluation.
For those with type 1 diabetes, weight management is still important but should be approached carefully under medical guidance, as insulin therapy can impact weight. A balanced diet and regular physical activity can help maintain a healthy weight and promote better blood sugar control.
Managing diabetes requires a comprehensive approach that includes a healthy diet, regular exercise, and maintaining a healthy weight. By incorporating these lifestyle changes, you can help control your blood sugar levels naturally and reduce the risk of complications. Whether you have type 1 or type 2 diabetes, these strategies can empower you to live a healthier, more balanced life.
Monitoring and Managing Blood Sugar Levels
Effective blood sugar management is the cornerstone of diabetes control, helping to prevent complications and maintain a healthy lifestyle. Monitoring your blood sugar levels regularly allows you to adjust your diet, exercise, and medications accordingly. This section outlines how to monitor blood sugar effectively and why it’s so important for diabetes management.
How to Manage Blood Sugar Levels
Monitoring blood sugar levels helps you understand how your body responds to different foods, activities, and medications. Consistent monitoring can help prevent both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar), which are crucial for preventing long-term complications.
- Home Glucose Meters: These devices allow you to check your blood sugar levels at home. After pricking your finger with a lancet, a drop of blood is placed on a test strip and inserted into the meter. This gives you a reading of your blood sugar levels within seconds. It’s quick, easy, and essential for tracking daily fluctuations in blood sugar.
- Continuous Glucose Monitors (CGMs): CGMs are more advanced devices that continuously monitor blood sugar levels throughout the day and night. A small sensor placed under the skin tracks glucose levels in real-time, sending data to a receiver or smartphone app. CGMs provide a more comprehensive picture of blood sugar patterns and are especially useful for people with type 1 diabetes or those needing intensive glucose monitoring.
Importance of Regular Blood Sugar Monitoring
Regular blood sugar monitoring is vital for keeping your diabetes under control and preventing complications. By tracking your glucose levels:
- Adjust Medications: Monitoring allows you to adjust insulin doses or oral medications based on your readings. This is essential for keeping blood sugar within the target range.
- Prevent Complications: Keeping blood sugar levels stable reduces the risk of serious complications such as heart disease, kidney damage, nerve damage, and vision loss. Consistent monitoring helps catch high or low blood sugar early, preventing these complications from worsening.
- Manage Lifestyle Choices: Blood sugar levels fluctuate in response to food, exercise, stress, and sleep. Monitoring helps you understand how these factors affect your glucose levels, allowing you to make more informed decisions about your lifestyle.
How Often Should You Monitor?
The frequency of monitoring depends on the type of diabetes you have and your treatment plan:
- Type 1 Diabetes: Frequent monitoring is recommended, especially if you’re using insulin. You may need to check your blood sugar several times a day.
- Type 2 Diabetes: If you’re managing diabetes through diet, exercise, and oral medications, you may only need to monitor once or twice a day. Those using insulin may need more frequent checks.
- Gestational Diabetes: Blood sugar monitoring is critical during pregnancy to ensure both maternal and fetal health. Monitoring is typically done multiple times a day, especially after meals.
Regular and effective blood sugar monitoring is a vital part of diabetes management. It empowers you to take control of your condition, make timely adjustments to your care plan, and minimize the risk of complications. Whether using a home glucose meter or a continuous glucose monitor, staying on top of your blood sugar levels is key to living well with diabetes.
Prevention of Diabetes and Related Complications
Preventing diabetes, particularly type 2 diabetes, and managing the complications that arise from poorly controlled diabetes is essential for long-term health. Although type 1 diabetes cannot be prevented, many lifestyle interventions can help prevent type 2 diabetes and its associated complications. This section covers actionable steps to prevent diabetes and manage its complications effectively.
Preventing Type 2 Diabetes
Type 2 diabetes is often preventable through healthy lifestyle choices. For those at high risk, including individuals with prediabetes, early interventions can significantly reduce the chances of developing full-blown diabetes. Here are the key steps:
- Healthy Diet: Adopting a balanced, nutrient-rich diet is crucial for preventing type 2 diabetes. Focus on whole grains, fruits, vegetables, lean proteins, and healthy fats. Avoid sugary beverages, processed foods, and refined carbohydrates that can spike blood sugar levels.
- Regular Exercise: Physical activity plays a major role in maintaining healthy blood sugar levels and reducing insulin resistance. Aim for at least 150 minutes of moderate exercise per week, such as brisk walking, cycling, or swimming. Incorporating resistance training can further help improve insulin sensitivity.
- Weight Management: Being overweight or obese is a significant risk factor for developing type 2 diabetes. Losing even 5-10% of body weight can reduce the risk of diabetes by improving insulin sensitivity and lowering blood sugar levels.
- Early Intervention in Prediabetes: Individuals diagnosed with prediabetes have higher-than-normal blood sugar levels but are not yet in the diabetic range. Early lifestyle changes, such as improving diet and increasing physical activity, can reverse prediabetes and prevent the progression to type 2 diabetes.
Preventing Diabetes Complications
For those already diagnosed with diabetes, preventing complications is critical for maintaining quality of life. Proper management of blood sugar levels, along with routine medical care, can prevent or delay the onset of severe health issues related to diabetes.
- Manage Blood Sugar Levels: Consistently maintaining blood sugar within the target range is crucial to avoid long-term complications. Follow your diabetes treatment plan closely, whether it involves medications, insulin therapy, or lifestyle adjustments.
- Foot Care: Diabetes can lead to nerve damage (diabetic neuropathy), making foot injuries difficult to detect. Untreated wounds can develop into serious infections. Regularly inspect your feet for sores, blisters, or cuts, and keep them clean and dry. Seek immediate medical attention if you notice any foot injuries that don’t heal.
- Eye Health: Diabetic retinopathy, caused by damage to the blood vessels in the retina, is a leading cause of vision loss in people with diabetes. Regular eye exams are essential for detecting early signs of eye problems. Managing blood sugar, blood pressure, and cholesterol levels can also help protect your eyes.
- Kidney Health: High blood sugar can damage the kidneys over time, leading to diabetic nephropathy. To prevent kidney complications, monitor your blood pressure, maintain a healthy diet, and avoid excessive use of non-steroidal anti-inflammatory drugs (NSAIDs), which can stress the kidneys.
- Heart Health: Diabetes significantly increases the risk of heart disease and stroke. To protect your heart, keep your blood pressure and cholesterol levels in check through a heart-healthy diet, regular exercise, and, if needed, medications prescribed by your healthcare provider.
- Regular Medical Checkups: Routine medical visits help you stay on top of potential diabetes-related complications. Regular screenings for kidney function, eye health, and cardiovascular health are essential. These checkups allow for early intervention if any issues arise, reducing the likelihood of serious complications.
By adopting these preventive measures, individuals can greatly reduce their risk of developing type 2 diabetes and prevent complications related to both type 1 and type 2 diabetes. Taking control of your lifestyle and working closely with healthcare professionals is key to living a healthier life with diabetes.
Frequently Asked Questions (FAQs)
Here are some of the most commonly asked questions about diabetes, providing clear answers to help you understand the condition better.
Q: Is diabetes genetic?
A: Genetics can influence both type 1 and type 2 diabetes, but the role of genes varies. Type 1 diabetes has a stronger genetic link, while type 2 diabetes is often associated with lifestyle factors such as diet, exercise, and weight, though genetics can still play a role.
Q: Can diabetes be cured?
A: Currently, there is no cure for diabetes. However, type 2 diabetes can sometimes be put into remission through significant lifestyle changes like weight loss, healthy eating, and exercise. Type 1 diabetes requires lifelong insulin management and cannot be cured.
Q: What is insulin resistance?
A: Insulin resistance occurs when the body’s cells no longer respond effectively to insulin, causing elevated blood sugar levels. This condition is a precursor to type 2 diabetes and is often associated with obesity and sedentary lifestyles.
Q: What is prediabetes?
A: Prediabetes is a condition where blood sugar levels are higher than normal but not yet high enough to be classified as type 2 diabetes. Without intervention, prediabetes often progresses to diabetes, but lifestyle changes can help reverse it.
Q: What happens if diabetes is untreated?
A: If left untreated, diabetes can lead to serious health complications such as heart disease, kidney damage, nerve damage, vision loss, and increased risk of infections. Early diagnosis and management are key to preventing these complications.
Q: What are the early symptoms of diabetes?
A: Common early symptoms include frequent urination, excessive thirst, unexplained weight loss, fatigue, blurred vision, and slow-healing sores. If you experience these, it’s important to consult a healthcare provider for evaluation.
Q: Can you prevent type 2 diabetes?
A: Yes, type 2 diabetes can often be prevented or delayed with healthy lifestyle choices such as maintaining a healthy weight, staying active, and following a balanced diet low in processed sugars and fats.
Q: Is insulin always needed for type 2 diabetes?
A: Not always. Many people with type 2 diabetes can manage their blood sugar with lifestyle changes, oral medications, or non-insulin injectable drugs. However, some may eventually require insulin as the condition progresses.
Q: Can diabetes cause weight loss?
A: Unexplained weight loss is more common in type 1 diabetes but can occur in type 2 diabetes as well. It’s a sign that the body isn’t using glucose effectively, leading to fat and muscle breakdown for energy.
Q: How often should people with diabetes check their blood sugar?
A: The frequency of blood sugar checks depends on the type of diabetes, treatment regimen, and overall blood sugar control. Type 1 diabetics or those using insulin may need to check multiple times a day, while others might check less frequently. Your doctor can advise the best schedule.
Conclusion
In conclusion, understanding diabetes is crucial for effective prevention and management. The three main types of diabetes—type 1, type 2, and gestational diabetes—differ in their causes and treatment approaches, but they all share the challenge of regulating blood sugar levels. Recognizing the causes and symptoms of diabetes, such as frequent urination, excessive thirst, and unexplained weight loss, allows for early detection, which is key to preventing serious complications like heart disease, nerve damage, and kidney failure.
Proper management through lifestyle changes, including a healthy diet, regular exercise, and consistent blood sugar monitoring, plays a significant role in controlling diabetes. Although diabetes cannot be cured, it can be effectively managed, and in some cases, type 2 diabetes may even be reversed with the right interventions.
For those concerned about their risk or already living with diabetes, consulting healthcare professionals is essential for personalized advice. With the right guidance and commitment to lifestyle adjustments, many complications can be avoided, and a healthy, active life is entirely possible.

